The rural state of New Hampshire has some of the lowest HIV incidence and prevalence rates in the United States. That's great news, but it comes with a price.
Many at risk people in New Hampshire think HIV is a third world or city problem and not something they need to worry about personally. That means they are less likely to take precautions against HIV.
At the same time, people who have been diagnosed with HIV in New Hampshire face stigma from neighbors and friends who may be less familiar with HIV than people living in urban areas where the disease is more prevalent. Geography adds to those challenges: the ~650 people cared for at Dartmouth-Hitchcock HIV Program come from a much wider geographic area than patients in similarly sized clinics in metropolitan areas. That translates to longer travel times and more complicated access to care.
Not surprisingly, HIV patients living in rural areas have been shown by Sam Bozzette and others to receive substandard care, probably because HIV experts are not sufficiently accessible.
In formal analyses at the Dartmouth-Hitchcock HIV Program, our HIV expert providers delivered outstanding care equivalently to rural and urban patients But despite this my colleagues and I showed that our rural patients have higher rates of depression and even higher mortality. New Hampshire might be a lovely place to live, but living with HIV infection anywhere is no walk in the park.
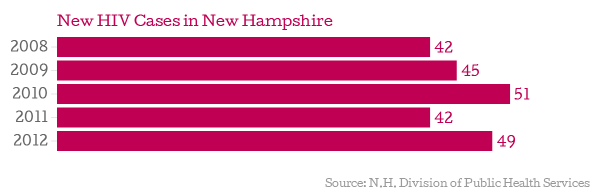
Todd Bookman of NHPR touches on these and other issues in nice radio story in which I was quoted. There are still plenty of battles remaining in the war against HIV in New Hampshire.

![[ M U R M U R S ]](http://images.squarespace-cdn.com/content/v1/51efa33ce4b09afa04cb2a66/1376911411704-LDY4UEIH1WRGPUXTMLJU/Logo.jpg?format=1500w)